The Language of Stem Cell Medicine: What are They? What Makes Them so Special? And What do all Those Acronyms Mean?
SUNDAY, 28 AUGUST 2016 / PUBLISHED IN BLO
Stem cell medicine leverages the body’s innate ability to heal itself, offering alternatives to conventional drugs and invasive surgeries. Stem cell therapies involve engineering human stem cells to repair or restore damaged organs and tissues, aiming to reinstate normal function.
Types of Stem Cell Therapies
Stem cell therapies encompass a range of approaches, including progenitor cells like those used in bone marrow transplants and cellular products such as platelet-rich plasma (PRP). While PRP and progenitor cells have been extensively used in clinical settings, stem cell therapies are rapidly advancing to address various medical conditions.
Autologous vs. Allogeneic Stem Cells

Stem cell treatments typically fall into two categories:
Autologous Stem Cells
Derived from the patient’s own body, autologous stem cells are used exclusively for the patient’s benefit. This approach minimizes the risk of rejection and allows for immediate treatment without the need for donor matching. Common sources include bone marrow and adipose tissue, facilitating therapies ranging from orthopedic conditions to wound healing.
Allogeneic Stem Cells
Harvested from donors, allogeneic stem cells undergo rigorous testing for diseases and are often cultured to increase cell counts. These stem cells, regulated under strict FDA guidelines, hold potential for large-scale production and widespread therapeutic applications across diverse patient populations.
Understanding Stem Cell Types
Adult Stem Cells (ASCs)
Found in various tissues, adult stem cells replenish dying cells and regenerate tissues like bone, cartilage, and adipose tissue. Over 2,000 clinical trials worldwide have explored their therapeutic potential, primarily from bone marrow and adipose tissue sources.
Induced Pluripotent Stem Cells (iPSCs)
Derived from adult cells, iPSCs are genetically reprogrammed to exhibit pluripotency, meaning they can differentiate into any cell type. Despite their versatility, iPSCs carry higher risk profiles compared to adult and embryonic stem cells.
Embryonic Stem Cells (ESCs)
Derived from human embryos, embryonic stem cells are a subject of ethical debate but remain vital for understanding regenerative processes and advancing medical research.
Types of Adult Stem Cells
Bone Marrow Stem Cells

First identified in bone marrow, these stem cells play crucial roles in healing bones and replacing blood cell types. FDA-approved under specific conditions, their use requires meticulous lab cultivation and regulatory oversight.
Adipose-Derived Stem Cells
Discovered in fat tissues, adipose-derived stem cells (ADSCs) can differentiate into diverse cell types, revolutionizing fields from plastic surgery to regenerative medicine.
- Published in Blog
Adipose Stem Cell Therapies are Revolutionizing Plastic Surgery, and Demand is High
THURSDAY, 25 AUGUST 2016 / PUBLISHED IN BLOG
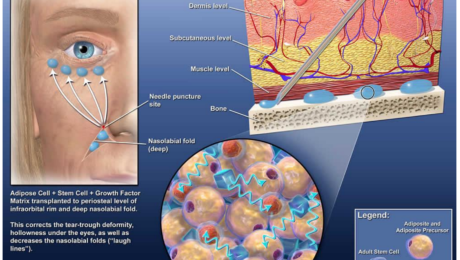
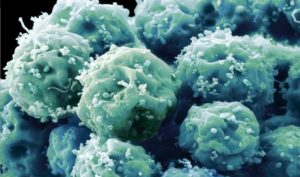
Adipose stem cells (pictured) harvested from body fat. (Photo: Genetic Engineering & Biotechnology News).
Introduction to Adipose Stem Cells
The discovery of abundant stem cell populations in body fat tissue changed everything the medical community thought it knew about stem cells overnight. Now, adipose stem cell therapies are driving the plastic and cosmetic surgery industries, and demand among patients keeps rising.
Discovery of Adipose Stem Cells
In 2001, researchers and plastic surgeons from the University of Pittsburgh discovered that human fat tissue is a very rich source of mesenchymal stem cells (MSCs), multipotent stromal cells that can differentiate into a variety of cell types. When their findings were published in the Tissue Engineering Journal, the discovery stirred quite an epiphany in the medical and scientific community—until then, adult MSCs were predominantly believed to be strictly a bone marrow product. Little did those researchers realize at the time that their discovery would revolutionize cosmetic surgery in less than a decade.
Advantages of Adipose Tissue Over Bone Marrow
Adipose tissue offers distinct advantages over bone marrow tissue. Adipose fat is easier to extract than bone marrow, and the stem cell population contained in fat tissue is far more abundant than in bone marrow. One ounce of fat contains 300-500 times as many mesenchymal stem cells as an ounce of bone marrow. And unlike bone marrow, because of autologous adipose tissue’s copious stem cell count, most procedures using them do not require cells to be expanded in a lab, which means that most adipose stem cell therapies can be performed in the same operative procedure. Because bone marrow typically needs to be culture expanded for days in a lab before they can be re-injected back into a patient and adipose cells do not, there are plenty of advantages to adipose stem cell therapies.
Adipose Stem Cell Therapy Procedures

Over the past 10 years, plastic surgeons have established safe and convenient ways to remove fat and isolate the stem cells for use in cosmetic procedures. And since adipose stem cells are extracted and reintroduced to the patient’s own body, the risk of rejection that goes with donor stem cells is eliminated. Scores of ongoing clinical trials using adipose stem cells have already proven their safety and efficacy in a variety of applications. Anti-aging therapies using adipose stem cells, for instance, have grown exponentially in popularity.
Anti-Aging Benefits of Adipose Stem Cells

Cosmetic cell assisted fat transfer
As we age, cells become progressively damaged over time from sun, toxins in the environment, and the natural loss of moisture that keeps youthful skin full and wrinkle-free. Adipose stem cells work to regenerate and repair that damaged tissue, and adjunctive treatments can potentially slow down or reverse the aging process. Those cells possess a unique anti-aging effect by means of regenerating and repairing organs—including skin—damaged by environmental elements we are exposed to in our daily life, and by improving immune functions.
International Demand for Stem Cell Anti-Aging Therapies
This discovery has created an international demand for stem cell anti-aging therapies, which since these procedures are non-invasive (no surgery involved), make for a faster recovery and significantly less downtime for patients. Many patients and physicians feel that adipose stem cells also create a more natural appearance for recipients than traditional cosmetic surgery procedures. Some cosmetic stem cell physicians have taken it up a notch with cell-assisted fat transfer, in which autologous adipose-derived (stromal) stem cells are used in combination with lipoinjection for even softer, more natural results.
Procedure of Cell-Assisted Fat Transfer
Here’s how it works: a stromal vascular fraction (SVF) containing ASCs is freshly isolated from half of the aspirated fat and recombined with the other half. This process converts relatively ASC-poor aspirated fat to ASC-rich fat, reducing the potential for postoperative atrophy of injected fat to a minimal level, which clinical trials have found does not change substantially after two months.
Adipose Tissue as a Regenerative Therapy
While adipose tissue is a definitive source of stem cells, what if you don’t need to isolate or separate the stem cells to benefit from their regenerative powers?

Radiation to treat a tumor severely affected this boy’s facial growth and development, caused significant facial asymmetry and left a large cosmetic defect on the side of his head. Fat grafting surgery restored his appearance to that of any healthy, happy, 14-year-old.
Regenerative Properties of Fat Grafting
Plastic surgeons have known for years that fat grafting itself, without extracting the stem cells, has regenerative properties. Cosmetic surgeons have developed safe and predictable techniques for fat grafting and have documented the regenerative effects of fat grafting in different tissues, for a variety of conditions and diseases. Adipose stem cell-rich fat grafting has been documented to reverse radiation tissue damage, something that was considered irreversible until recently. Current clinical studies are documenting the regenerative effects of fat grafting in areas no one suspected, such as autoimmune diseases and degenerative joint disease. Unlike bone marrow tissue, adipose tissue is easy to extract, it’s abundant, and it’s effective in ways researchers have only begun to discover. Cell-assisted fat grafting serves a valuable role in helping people with disfiguring injuries and birth defects.
Advancements in Adipose Tissue Applications
Plastic surgeons have acquired decades of experience in harvesting and refining adipose tissue for treating patients. Thanks to the remarkable level of expertise they have developed with adipose tissue, experts now play a leading role in developing its evolving regenerative applications. Regenerative medicine is changing the landscape of cosmetic and reconstructive surgery, and aesthetic medicine—and it keeps getting better!
- Published in Blog
Regenerating and Restoring Brain Cells in the Aged With Donor Neural Stem Cells
TUESDAY, 12 JULY 2016 / PUBLISHED IN BLOG
Introduction to Brain Plasticity and Aging
The human brain, as it turns out, is far more malleable than we once thought, even adult brains. However, they are subject to age-related diseases and disorders, such as dementia and diminished cognitive function. There is hope that medical science may be able to replace brain cells and restore memory in aging patients thanks to new discoveries in neural stem cell techniques.
New Techniques in Neural Stem Cell Research
Researchers at the Texas A&M Health Science Center College of Medicine recently published new findings in the journal Stem Cells Translational Medicine. These findings suggest a new technique for preparing donor neural stem cells and grafting them into an aged brain can regenerate tissue that has succumbed to structural, chemical, and functional changes, as well as a host of neurocognitive changes that can be attributed to aging.
Key Findings from the Study
The study, titled “Grafted Subventricular Zone Neural Stem Cells Display Robust Engraftment and Similar Differentiation Properties and Form New Neurogenic Niches in the Young and Aged Hippocampus,” was led by Ashok K. Shetty, Ph.D., a professor in the Department of Molecular and Cellular Medicine. Shetty is also the associate director of the Institute for Regenerative Medicine and a research career scientist at the Central Texas Veterans Health Care System.
Focus on the Aged Hippocampus
Shetty and his team at Texas A&M focus on the aged hippocampus, which plays an important role in making new memories and connecting them to emotions. They took healthy donor neural stem cells and implanted them into the hippocampus of an animal model, enabling them to regenerate tissue.
Significance of the Hippocampus
“We chose the hippocampus because it’s so important in learning, memory, and mood function,” Shetty said. “We’re interested in understanding aging in the brain, especially in the hippocampus, which seems particularly vulnerable to age-related changes.” The volume of this part of the brain decreases during the aging process, potentially related to a decline in neurogenesis (production of new neurons) and memory deficits.
Challenges in the Aged Hippocampus
The aged hippocampus exhibits signs of age-related degenerative changes, such as chronic low-grade inflammation and increased reactive oxygen species. Bharathi Hattiangady, assistant professor at the Texas A&M College of Medicine and co-first author of the study, was excited to discover that the aged hippocampus can accept grafted neural stem cells as well as the young hippocampus does, a discovery with significant implications for treating age-related neurodegenerative disorders.
Neural Stem Cell Grafting Process
In this new study, the team found that neural stem cells engrafted well onto the hippocampus in both young and older animal models. Not only did these implanted cells survive, but they also divided several times to create new cells. “They had at least three divisions after transplantation,” Shetty said. “The total yield of graft-derived neurons and glia was much higher than the number of implanted cells, in both the young and aged hippocampus.”
Creation of New Neural Stem Cell Niches

In both old and young brains, a small percentage of the grafted cells retained their stemness feature—an essential characteristic of a stem cell that distinguishes it from ordinary cells—and continuously produced new neurons. This process creates a new ‘niche’ of neural stem cells, which continue to produce new neurons at least three months after implantation.
Comparison to Previous Efforts
Past efforts to rejuvenate brains using fetal neurons were not as successful. Immature cells, such as neural stem cells, can tolerate the hypoxia (lack of oxygen) and trauma of the brain grafting procedure better than relatively mature neurons. The research team used a new technique of preparing the donor neural stem cells, leading to these promising results.
The Role of Brain Marrow
The researchers used donor cells from the sub-ventricular zone of the brain, an area called the “brain marrow,” analogous to bone marrow. This area holds a number of neural stem cells that persist throughout life, continuously producing new neurons that migrate to the olfactory system and respond to injury signals.
Potential of Induced Pluripotent Cells from Skin
Even a small stem cell sample can be expanded in culture, making the procedure minimally invasive. In the future, a single skin cell might suffice to create induced pluripotent stem cells, which can be pushed into neural stem cells. This eliminates the need to obtain cells from the brain, potentially revolutionizing the process.
Future Research Directions
Although the success of the grafted cells is promising, further research is needed to determine if the increased grey matter improves cognition. “Next, we want to test the impact of the implanted cells on behavior and determine if implanting neural stem cells can reverse age-related learning and memory deficits,” Shetty said. He is focused on rejuvenating the aged brain to promote successful aging, maintaining normal cognitive function, and the ability to make memories.
- Published in Blog
Stem Cell “Tattoo” Technology Allows Researchers to Track Cell Implants Non-invasively
TUESDAY, 12 JULY 2016 / PUBLISHED IN BLOG
Introduction to Stem Cell Tattoo Technology
Researchers at the University of Toronto have developed a tracer ink—a “stem cell tattoo”—that provides the ability to monitor stem cells in unprecedented detail after they’re injected. The research findings, titled “Bifunctional Magnetic Silica Nanoparticles for Highly Efficient Human Stem Cell Labeling,” were published in June in the Journal of Magnetic Resonance Imaging. Already emerging as an ideal probe for noninvasive cell tracking, the technology has the potential to revolutionize stem cell research by arming scientists with the ability to visually follow the pathways and effectiveness of stem cell therapies in the body in real time.
Advancements in Stem Cell Tracking
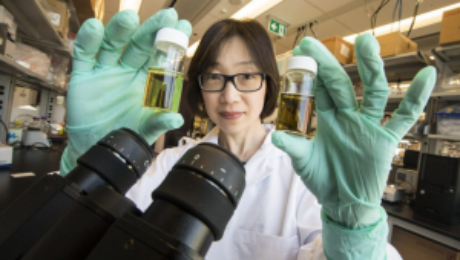
University of Toronto biomedical engineering professor Hai-Ling Margaret Cheng, a biomedical engineer who specializes in medical imaging, says the new technology allows researchers to actually see and track stem cells after they’re injected. Cheng hopes the technique will help expedite the development and use of stem cell therapies.
Development of the Contrast Agent
Working with colleague Xiao-an Zhang, an assistant professor of chemistry at the University of Toronto, Scarborough, Cheng developed a singular chemical compound known as a contrast agent that acts as a tracer. Composed of manganese, an element that naturally occurs in the body, this tracer compound, called MnAMP, bathes stem cells in a green solution, rendering them traceable inside the body under MRI.
Long-term Cell Tracking with Tracer Ink
The contrast agent “ink” first enters a stem cell by penetrating its membrane. Once inside, it stimulates a chemical reaction that prevents it from seeping out of the cell the same way it entered. Previous versions of contrast agents easily escaped cells. By establishing a way to contain the ink within the cell’s walls, the research team achieved the ability to track the cells long term once they are inside the body.
Advantages of the New Technology
According to Cheng, some basic contrast agents are already available for use in humans, but none are capable of tracking cells over a long period of time. Contrast agents work by illuminating the deepest and darkest corners of a person’s internal architecture so they appear clearly under X-rays, computed tomography (CT) scans, and MRIs. An example of a currently used contrasting agent would be the barium sulfate solution given to patients to help diagnose certain disorders of the esophagus, stomach, or intestines.
Non-invasive Cell Tracking Benefits
Before the stem cell tattoo tracer ink was developed, surgery was the only option for scientists to get a literal glance of a cell’s destiny after it was injected into the body. Now, researchers can track the results in real time without resorting to any invasive procedures. “Before, we could not visually track the cells once they were introduced into the body,” Cheng says. “Now we have the ability to view cells in a non-invasive manner using MRI, and monitor them for potentially a very long time.”
Current Stage of Development

Currently, the tracer ink technology is still in the early development phase and requires more animal testing. Cheng is hopeful it can proceed to human clinical trials in about 10 years. While Cheng has already proven that tattooing an animal’s embryonic stem cell doesn’t affect its ability to transform into a functional heart cell, larger models, such as rats or pigs (which better represent human size), are up for evaluation next.
Future Testing and Applications
In those test cases, researchers will cut off and reduce blood flow in the animals to mimic the effects of damage caused by a human heart attack. Cardiac stem cells pre-tagged with Cheng’s ink tracer technology will then be injected into the damaged tissue. Using MRI to monitor the luminous inked stem cells in action, researchers can non-invasively follow where in the body they’re traveling and more easily determine if the new cells are responsible for restoring normal heart rhythm. Before it can be tested in humans, the chemical tracer will also have to pass rigorous toxicology tests to ensure its safety.
- Published in Blog
Stem Cell-stimulating Fillings Help Regenerate Teeth Damaged by Disease, Decay
MONDAY, 11 JULY 2016 / PUBLISHED IN BLOG
Introduction to Stem Cell-stimulating Fillings
Researchers from Harvard University and the University of Nottingham have developed a new filling that stimulates stem cells in dental pulp to regenerate and even regrow teeth damaged by disease and decay. According to Newsweek Magazine, the discovery earned a prize from the Royal Society of Chemistry after judges described it as a “new paradigm for dental treatments.” The treatment is believed to potentially eliminate the need for root canals.
How the Filling Material Works
The filling works by stimulating the body’s natural store of stem cells to encourage the growth of dentin—the bony material that makes up the majority of the tooth—allowing patients to effectively regrow teeth that are damaged through dental disease. The filling’s synthetic biomaterials are used similarly to dental fillings, placed in direct contact with pulp tissue in the damaged tooth. This stimulates the tissue’s native stem cell population to repair and regenerate pulp tissue and the surrounding dentin.
Comparison to Current Dental Treatments
The discovery is a significant step forward from current methods to treat cavities, which involve drilling out decay and putting in a filling made of gold; porcelain; silver amalgam (which consists of mercury mixed with silver, tin, zinc, and copper); or tooth-colored plastic or composite resin. When these fillings fail to halt the tooth’s decay, a root canal is needed to remove the pulp of the tooth, damaging it even further.
Potential for Industry Adoption
Researchers hope to develop the technique with industry partners to make it available for dental patients as an alternative to traditional fillings. Marie Curie research fellow Adam Celiz says that existing dental fillings are toxic to cells and are therefore incompatible with pulp tissue inside the tooth. “In cases of dental pulp disease and injury, a root canal is typically performed to remove the infected tissues,” Celiz says.
Recognition and Awards
The promise of using therapeutic biomaterials to bring stem cell medicine to restorative dentistry could significantly impact millions of dental patients each year. The approach is so promising it won second prize in the materials category of the Royal Society of Chemistry’s Emerging Technology Competition for 2016. Competition entries were judged on the degree of innovation of the technology, its potential impact, and the quality of the science behind it.
Future of Dentistry with Stem Cell Technology
The stem cell-stimulating filling promises to change the future of dentistry, according to David Mooney, Pinkas Family Professor of Bioengineering at the John Paulson School of Engineering and Applied Sciences at Harvard and the Wyss Institute for Biologically Inspired Engineering. “These materials may provide an effective and practical approach to allow a patient to regenerate components of their own teeth,” Mooney says.
Broader Implications of Stem Cell Research
Stem cells can induce regenerative, self-healing qualities in any tissue found in the body and can, as a result, provide unlimited potential for medical applications. Current studies are underway worldwide to learn how stem cells may be used to prevent or cure diseases and injuries such as Parkinson’s disease, type 1 diabetes, heart disease, spinal cord injury, muscular dystrophy, Alzheimer’s disease, strokes, burns, osteoarthritis, vision and hearing loss, and more. Stem cells may also be used to replace or repair tissue damaged by disease or injury
- Published in Blog
What are the potential uses of human stem cells? What obstacles must still be overcome before these potential uses will be realized?
TUESDAY, 28 JUNE 2016 / PUBLISHED IN BLOG
Introduction to Human Stem Cells and Their Potential Uses
There are many ways in which human stem cells can be used in research and in the clinic. Studies of stem cells continue to yield information about their complex capabilities. A primary goal of this research is to identify how undifferentiated stem cells become the differentiated cells that form the tissues and organs. Scientists know that turning genes on and off is central to this process. Some of the most serious medical conditions, such as cancer and birth defects, are due to abnormal cell division and differentiation.
Understanding Genetic and Molecular Triggers
A more complete understanding of the genetic and molecular triggers of these conditions can yield information about how they arise and suggest new strategies to treat them. Predictably controlling cell proliferation and differentiation requires additional basic research on the molecular and genetic signals that regulate cell division and specialization. While recent developments with induced pluripotent stem cells (iPSCs) suggest some of the specific factors that may be involved, techniques must be developed to introduce these factors safely into the cells and control the processes that are induced by these factors.
Human Stem Cells and Drug Testing
Human stem cells are also being used to test new drugs. New medications are tested for safety on differentiated cells generated from human pluripotent cell lines. Other kinds of cell lines have a long history of being used in this way. Cancer cell lines, for example, are used to screen potential anti-tumor drugs. The availability of pluripotent stem cells would allow drug testing on a wider range of cell types. However, to screen drugs effectively, the conditions must be identical when comparing different drugs. Therefore, scientists must be able to precisely control the differentiation of stem cells into the specific cell type on which drugs will be tested.
Challenges in Drug Testing with Stem Cells
For some cell types and tissues, current knowledge of the signals controlling differentiation falls short of being able to mimic these conditions precisely to generate pure populations of differentiated cells for each drug being tested.
Human Stem Cells in Cell and Tissue Generation

Perhaps the most important potential application of human stem cells is the generation of cells and tissues that could be used for cell-based therapies. Today, donated organs and tissues are often used to replace ailing or destroyed tissue, but the need for transplantable tissues and organs far outweighs the available supply. Stem cells, directed to differentiate into specific cell types, offer the possibility of a renewable source of replacement cells and tissues to treat diseases including macular degeneration, spinal cord injury, stroke, burns, heart disease, diabetes, osteoarthritis, and rheumatoid arthritis.
- Published in Blog
Mending a Broken Heart and Addressing Diabetes with Adult Stem Cells
TUESDAY, 28 JUNE 2016 / PUBLISHED IN BLOG
Introduction to Stem Cell Research for Heart Disease and Diabetes
Researchers are learning about mending a broken heart–that is, how to generate healthy heart muscle stem cells in the laboratory and then transplant those cells into patients with chronic heart disease. Preliminary research in mice and other animals indicates that bone marrow stromal cells, transplanted into a damaged heart, can have beneficial effects. Whether these cells can generate heart muscle cells or stimulate the growth of new blood vessels that repopulate the heart tissue, or help through some other mechanism is actively under investigation.
Stem Cell Research: Mending a Broken Heart
For example, injected cells may accomplish repair by secreting growth factors, rather than actually incorporating into the heart. Promising results from animal studies have served as the basis for a small number of exploratory studies in humans. Other recent studies in cell culture systems indicate that it may be possible to direct the differentiation of adult bone marrow cells into heart muscle cells.
Can Stem Cells Mend a Broken Heart?
For that matter, what can stem cells do to treat all cardiovascular diseases including hypertension, coronary heart disease, stroke, and congestive heart failure? Cardiovascular disease (CVD) has ranked the number one cause of death in the United States every year since 1900 except 1918, when the nation struggled with an influenza epidemic. Nearly 2,600 Americans die of CVD each day—roughly one person every 34 seconds. Given the country’s large aging population and the relatively dramatic recent increases in the prevalence of cardiovascular risk factors such as obesity and type 2 diabetes, CVD will be a significant health concern for decades to come.
Strategies to Treat Heart Disease with Stem Cells
Cardiovascular disease can deprive heart tissue of oxygen, thereby killing cardiac muscle cells (cardiomyocytes). This loss triggers a cascade of detrimental events, including formation of scar tissue, an overload of blood flow and pressure capacity, the overstretching of viable cardiac cells attempting to sustain cardiac output leading to heart failure, and eventual death. Restoring damaged heart muscle tissue, through repair or regeneration, is therefore a potentially new strategy to treat heart failure.
Research on Adult-Derived Stem Cells for Cardiac Repair
The use of adult-derived stem cells for cardiac repair is an active area of research. A number of stem cell types, including cardiac stem cells that naturally reside within the heart, myoblasts (muscle stem cells), adult bone marrow-derived cells including mesenchymal cells (bone marrow-derived cells that give rise to tissues such as muscle, bone, tendons, ligaments, and adipose tissue), endothelial progenitor cells (cells that give rise to the endothelium, the interior lining of blood vessels), and umbilical cord blood cells, have been investigated as possible sources for regenerating damaged heart tissue. All have been explored in mouse or rat models, and some have been tested in larger animal models, such as pigs.
Human Studies on Cardiac Repair with Stem Cells
A few small studies have also been carried out in humans, usually in patients who are undergoing open-heart surgery. Several of these have demonstrated that stem cells that are injected into the circulation or directly into the injured heart tissue appear to improve cardiac function and/or induce the formation of new capillaries. The mechanism for this repair remains controversial, and the stem cells likely regenerate heart tissue through several pathways. However, the stem cell populations that have been tested in these experiments vary widely, as do the conditions of their purification and application. Although much more research is needed to assess the safety and improve the efficacy of this approach, these preliminary clinical experiments show how stem cells may one day be used to repair damaged heart tissue, thereby reducing the burden of cardiovascular disease.
Treating Type I Diabetes with Stem Cells
In people who suffer from type 1 diabetes, the cells of the pancreas that normally produce insulin are destroyed by the patient’s own immune system. New studies indicate that it may be possible to direct the differentiation of human embryonic stem cells in cell culture to form insulin-producing cells that eventually could be used in transplantation therapy for persons with diabetes.
Steps for Successful Cell-Based Treatments
To realize the promise of novel cell-based therapies for such pervasive and debilitating diseases, scientists must be able to manipulate stem cells so that they possess the necessary characteristics for successful differentiation, transplantation, and engraftment. The following is a list of steps in successful cell-based treatments that scientists will have to learn to control to bring such treatments to the clinic. To be useful for transplant purposes, stem cells must be reproducibly made to:
- Reproduce extensively and generate sufficient quantities of cells for making tissue.
- Differentiate into the desired cell type(s).
- Survive in the recipient after transplant.
- Integrate into the surrounding tissue after transplant.
- Function appropriately for the duration of the recipient’s life.
- Avoid harming the recipient in any way.
Avoiding Immune Rejection in Stem Cell Therapies
Also, to avoid the problem of immune rejection, scientists are achieving good results with strategies that use the patient’s own stem cells to generate tissue that will not be rejected.
- Published in Blog
Stem Cell Myths, Busted
THURSDAY, 02 JUNE 2016 / PUBLISHED IN BLOG
Introduction to Stem Cell Myths and Facts
The term stem cell research gleans different reactions from people, both in the medical community and the wider public. Still an emerging science, stem cell research is shrouded by many myths and misconceptions. Here, we take on some of the most predominant myths to discuss the misconceptions and clarify the facts regarding this fast-growing branch of medicine.
Myth #1: Stem Cells Only Come from Embryos
FACT: False. Stem Cells Exist in All Bodies, from Embryos to Adults
Embryonic stem cells come from the early embryo and have the potential to produce all the specialized cells of the body. Because of this, they hold great promise for studying and potentially treating disease and injuries. Tissue or “adult” stem cells are found in the body throughout our lives. These cells maintain and repair many tissues in the body. Examples of these cells include blood stem cells, muscle stem cells, bone marrow stem cells, adipose tissue (fat) stem cells, and skin stem cells. Some of these adult stem cells are used in established medical and aesthetic treatments.
Myth #2: Induced Pluripotent Stem Cells (iPSCs) Eliminate the Need for Embryonic Cells
FACT: False. Research is Needed on All Types of Cells
It is not clear which cells will be most useful for which types of application. For the foreseeable future, side-by-side research on both embryonic and induced pluripotent stem cells is needed. Global Stem Cell Group’s research and treatment products use no embryonic stem cells.
Myth #3: Stem Cell Research Leads to Cloning Humans
FACT: False. Most Countries Prohibit Human Cloning

In most countries, even attempting to clone a human being is illegal. Some countries do allow something called “therapeutic cloning” for the purposes of studying a disease. In this procedure, scientists isolate embryonic stem cells from a cloned blastocyst (early stage embryo) but do not transfer the blastocyst into a womb. These stem cells are genetically matched to the donor organism for studying genetic disease. For example, stem cells could be generated using the nuclear transfer process described above, with the donor adult cell coming from a patient with diabetes or Alzheimer’s. The stem cells could be studied in the laboratory to help researchers understand what goes wrong in diseases like these. Therapeutic cloning also could be used to generate cells that are genetically identical to a patient’s. A patient transplanted with these cells would not suffer the problems associated with transplant rejection. To date, no human embryonic stem cell lines have been derived using therapeutic cloning.
Myth #4: Adult Stem Cells Are Only Found in Adults
FACT: False. Tissue Stem Cells Are Found in People of All Ages
There are three different types of stem cells: embryonic stem cells, induced pluripotent stem cells, and tissue-specific stem cells. It’s the tissue stem cells that are often called “adult” stem cells, but these “adult” stem cells are found in people of all ages.
Myth #5: Embryonic Stem Cell Research Is Banned in Europe
FACT: False. The Laws Vary Across the EU
EU member states have diverging regulatory positions on human embryonic stem cell research. For instance, in Germany, the use of embryos for research is heavily restricted under the Embryo Protection Act (Embryonenschutzgesetz) of 1991, which makes the derivation of embryonic stem cell lines a criminal offense. But in the UK, embryonic stem cell research is allowed, subject to licensing from the Human Fertilization and Embryology Authority (HFEA). Click here for country-by-country overviews for more details. Under the previous two European Framework programs (FP6 and F7), as well as the current program, Horizon 2020, human embryonic stem cell research can be funded, provided that the work is permitted by law in the country where it is to take place.
Myth #6: Stem Cell Research and Treatment Is Against the Law in the US
FACT: False. The FDA Regulates Stem Cell Products but They Are Not Illegal

The FDA does not regulate the practice of medicine, but rather drugs and medical devices and which of these can be marketed in the US. Under federal law, cultured (grown) stem cell products are considered a drug, but are not illegal. Adult stem cells, however, are not cultured—they exist in our bodies throughout our organs, blood, skin, teeth, fat, bone marrow, and other places. Adult stem cell therapy is currently used in the United States to treat conditions such as leukemia and other illnesses. Bone marrow consists of stem cells which have been transplanted for years in the US. Global Stem Cells Group offers stem cell treatments in countries where stem cell therapy is approved and regulated with no appreciable difference in safety record. Stem cell therapy technology is still under review by the FDA.
Myth #7: Bone Marrow Is the Best Source of Stem Cells
FACT: False. Bone Marrow Is Just One Source of Stem Cells
Bone marrow stem cells have been studied for decades and have been used to treat certain types of cancer. A great deal of research has been dedicated to understanding this source of stem cells and their potential. Bone marrow contains a number of different kinds of stem cells, one of which is mesenchymal stem cells. However, mesenchymal stem cells can also be found in adipose (fat) tissue at nearly 2000 times the frequency of bone marrow. Mesenchymal cells have the capability to become different types of tissues (blood vessels, muscle tissue, etc.) and are capable of communicating with other cells. In combination with other proteins, molecules, and regenerative cells found in adipose tissue, they also have the ability to reduce inflammation, regenerate damaged tissue, and grow new blood vessels, a process known as angiogenesis. Stem cells from adipose tissue are more accessible and abundant. They can be processed immediately and reintroduced into the body right away.
Myth #8: There Is a Risk of Rejection with Stem Cell Therapy
FACT: False. Autologous Stem Cells Eliminate the Risk of Rejection
When a patient’s stem cells are derived from his or her own body (such as fat tissue), there is no risk of rejection. In fact, studies thus far have indicated no safety issues with fat-derived autologous (from self) stem cells. Since these stem cells come from your own body, the risk of rejection is eliminated.
- Published in Blog
Stem Cell Treatments Normally Used for Cancer Patients are Helping Multiple Sclerosis Patients
MONDAY, 04 APRIL 2016 / PUBLISHED IN BLOG
Introduction
The British Broadcasting Corporation (BBC) recently reported that stem cell transplant treatments normally used for cancer patients are helping Multiple Sclerosis (MS) patients in the UK. According to the January 18, 2016 report, 20 patients received bone marrow stem cell transplants using their own stem cells, and at least some of the patients who were paralyzed by MS are able to walk again post-treatment.
Impact of Multiple Sclerosis in the UK
Approximately 100,000 people in the United Kingdom suffer from MS, with most new patients diagnosed between the ages of 20 and 30 years. “To have a treatment which can potentially reverse disability is really a major achievement,” says Prof Basil Sharrack of Sheffield’s Royal Hallamshire Hospital in Sheffield, England.
Autologous Hematopoietic Stem Cell Transplantation (HSCT)
The treatment, known as autologous hematopoietic stem cell transplantation (HSCT), involves the intravenous infusion of autologous or allogeneic stem cells harvested from the patient’s own bone marrow to reestablish hematopoietic function (formation of blood or blood cells) in patients whose bone marrow or immune system is damaged or defective by chemotherapy. Using stem cells harvested from the patient’s bone marrow helps rebuild the immune system. The theory is that these newly harvested cells are at such an early stage in development that the cellular defects that result in MS do not exist. “The immune system is being reset or rebooted back to a time point before it caused MS,” says Prof John Snowden, consultant hematologist at Royal Hallamshire Hospital.
Patient Success Stories
The BBC’s Panorama program spoke to several MS patients who have undergone the stem cell transplant. Steven Storey was diagnosed with MS in 2013 and, within a year, went from being an able-bodied athlete to wheelchair dependent and losing sensation in much of his body. “I went from running marathons to needing 24-hour acute care. At one point I couldn’t even hold a spoon and feed myself,” Storey says.

Clinical Trials and Research
The Royal Hallamshire Hospital along with hospitals in the United States, Sweden, and Brazil, is part of an international clinical trial called MIST that is assessing the long-term benefits of the stem cell procedure on MS patients. Study participants all have relapsing-remitting MS (RRMS) and received intensive chemotherapy to completely destroy the patients’ immune systems.
Cost and Accessibility of Treatment
Treatment costs are about the same as the annual cost for existing treatments, and the stem cell treatment does not require the use of new or existing medications. Prof Richard Burt of Northwestern University in Chicago carried out the first hematopoietic stem cell transplantation for MS in 1995, and is coordinating this current MIST international trial, which began in 2006. “There has been resistance to this in the pharma and academic world,” Burt says. “This is not a technology you can patent and we have achieved this without industry backing.”
Study Results and Future Implications
A study published last year involving MS patients in Chicago showed significant reductions in neurological disability, and for some, the improvements persisted for at least four years, although there was no comparative control group. The outcomes of the current international trial will be reported in 2018 and may determine whether the stem cell transplant becomes a standard in the United Kingdom’s healthcare system for many MS patients. “Ongoing research suggests stem cell treatments such as HSCT could offer hope, and it’s clear that in the cases highlighted by Panorama they’ve had a life-changing impact,” says Emma Gray, M.D., head of clinical trials at UK’s MS Society.
- Published in Blog